Kyphosis | Diagnosis & Treatments
How is kyphosis diagnosed?
Most cases of kyphosis are detected by parents, a pediatrician, or during a school screening. Early detection and follow-up are important for successful treatment. If your child has kyphosis, whether confirmed or suspected, they should be seen by an orthopedic specialist (orthopedist). The orthopedist will ask about your child’s medical and family histories, perform a physical exam, and measure the curve. They may order diagnostic tests to determine the nature and extent of your child’s kyphosis.
The first diagnostic test for kyphosis is usually an x-ray to measure and evaluate the degree of spinal curvature. This measurement will help determine what treatment your child needs to control or correct their kyphosis.
Other diagnostic testing might include:
- CT or CAT scan (computerized tomography scan), which uses a combination of x-rays and computer technology to produce cross-sectional images of the body with detailed images of bones, muscles, fat, and organs. Images from a CT scan are more detailed than images produced by an x-ray.
- MRI (magnetic resonance imaging) uses a combination of large magnets, radiofrequencies, and a computer to produce detailed images of organs and structures within the body. MRIs take longer than CT scans but produce more detailed images that can help identify or rule out spinal cord and nerve abnormalities.
- A bone scan is an imaging test that uses dye to identify any degenerative or arthritic changes in the joints, detect bone diseases and tumors, and determine the cause of bone pain or inflammation. It can also help identify or rule out infection or fractures.
- Blood tests are sometimes used to look for associated metabolic conditions. They are not a standard part of diagnosing kyphosis, however.
- Pulmonary function tests may be used to test your child’s lung function if their breathing is affected. This is not a standard part of diagnosing kyphosis, however.
How is kyphosis treated?
Kyphosis treatment depends on the complexity and severity, as well as your child’s age and stage of physical development.
The goals of kyphosis treatment are:
- to stop the progression of kyphosis in children who are still growing
- to prevent further deformity
- to correct spinal deformity in adolescents and young adults who have reached their full height
Non-surgical treatments for kyphosis
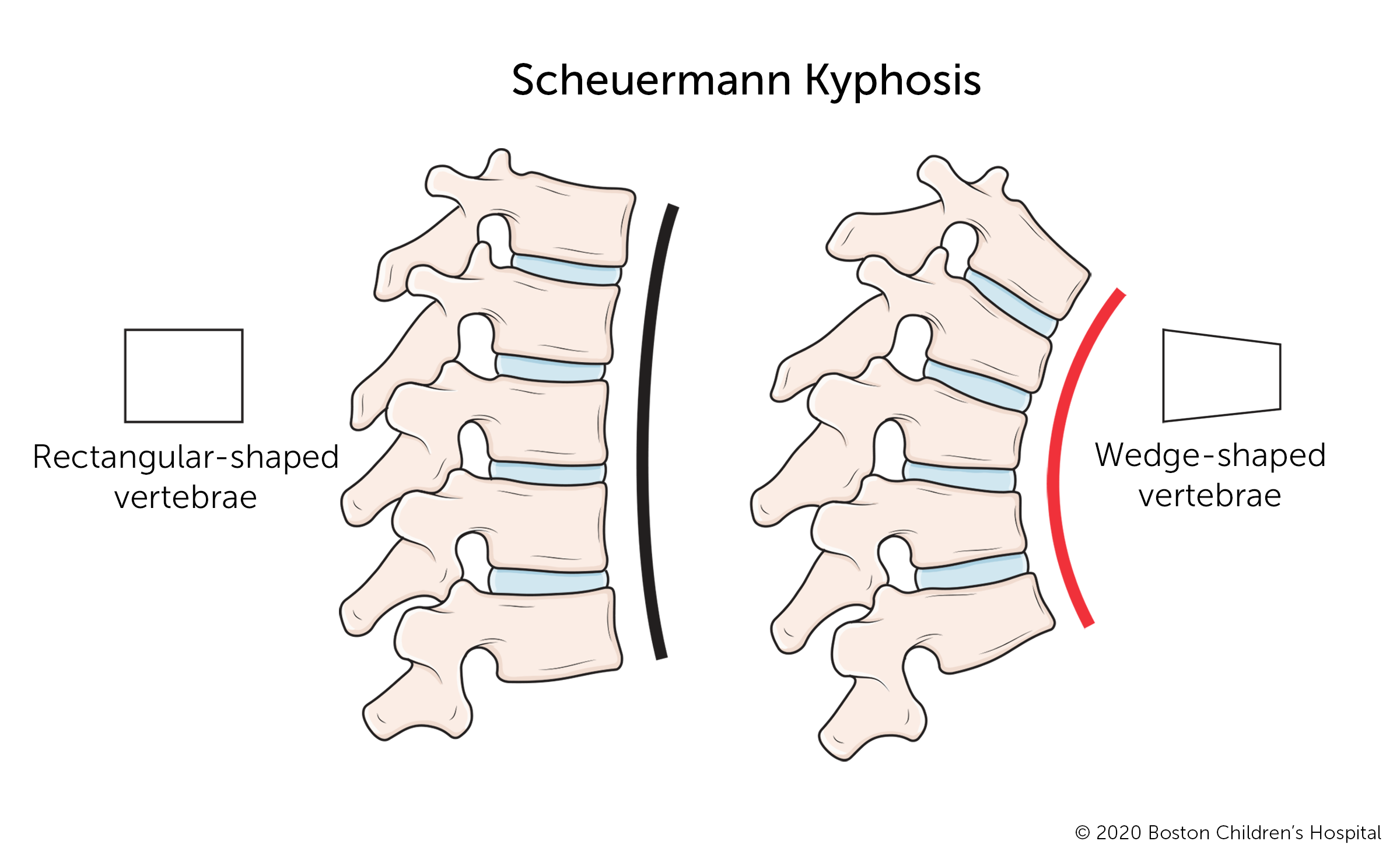
The majority of children with postural and Scheuermann’s kyphosis do not need aggressive treatment. Their treatment may include observation and monitoring, physical therapy, and possibly bracing.
Observation and monitoring
Even if your child is diagnosed with kyphosis, their spine may not curve any further. However, kyphosis can become more severe during periods of rapid growth. As your child grows, they need to be monitored through regular visits with an orthopedist. Their risk for developing severe kyphosis slows and eventually stops after puberty.
Physical therapy
Physical therapists provide exercise regimens and therapies to address the muscular imbalance associated with kyphosis. Exercises can help strengthen your child's core, upper back, shoulders, and shoulder blades.
Bracing
If your child has moderate or severe kyphosis and is at an early stage of growth, their doctor may prescribe a brace. Several factors will determine the most effective type of brace and amount of time your child should wear it, including the severity of their curve and their stage of growth. The brace holds your child's spine in a more upright position while they grow. This can partly correct the curve and prevent it from increasing.
- Bracing helps improve posture and function.
- Bracing can help control or correct curves.
- A successful bracing program may help your child avoid surgery.
The success of bracing depends on how well your child follows the custom regimen developed for them by their orthopedic doctor. Typical braces are the Boston Kyphosis brace (developed at Boston Children's Hospital) and the Milwaukee brace.
Surgical treatment for kyphosis
Spinal fusion surgery is the most common surgical procedure for treating severe cases of kyphosis. The surgeon will stabilize the curved section of the spine with instrumentation (rods and screws) and place bone grafts between the damaged vertebrae. This stimulates new bone growth so the vertebrae fuse into solid bone.
For young children who are still growing and require surgery, surgical options may include:
- Dual posterior growing rods (MAGEC rods) is a technique that uses extendable rods that are inserted into a child’s back to control the progression of spinal curvature. The rods are lengthened periodically to allow continued spinal growth.
- Expansion thoracostomy/VEPTR™ is a titanium rib implanted into a child’s back and chest to control the progression of chest and spinal deformity, while allowing growth of both the chest and the spine.
Your child may need kyphosis surgery if:
- their curve measures 75 degrees or more
- bracing proves unsuccessful at slowing or stopping the curve from progressing
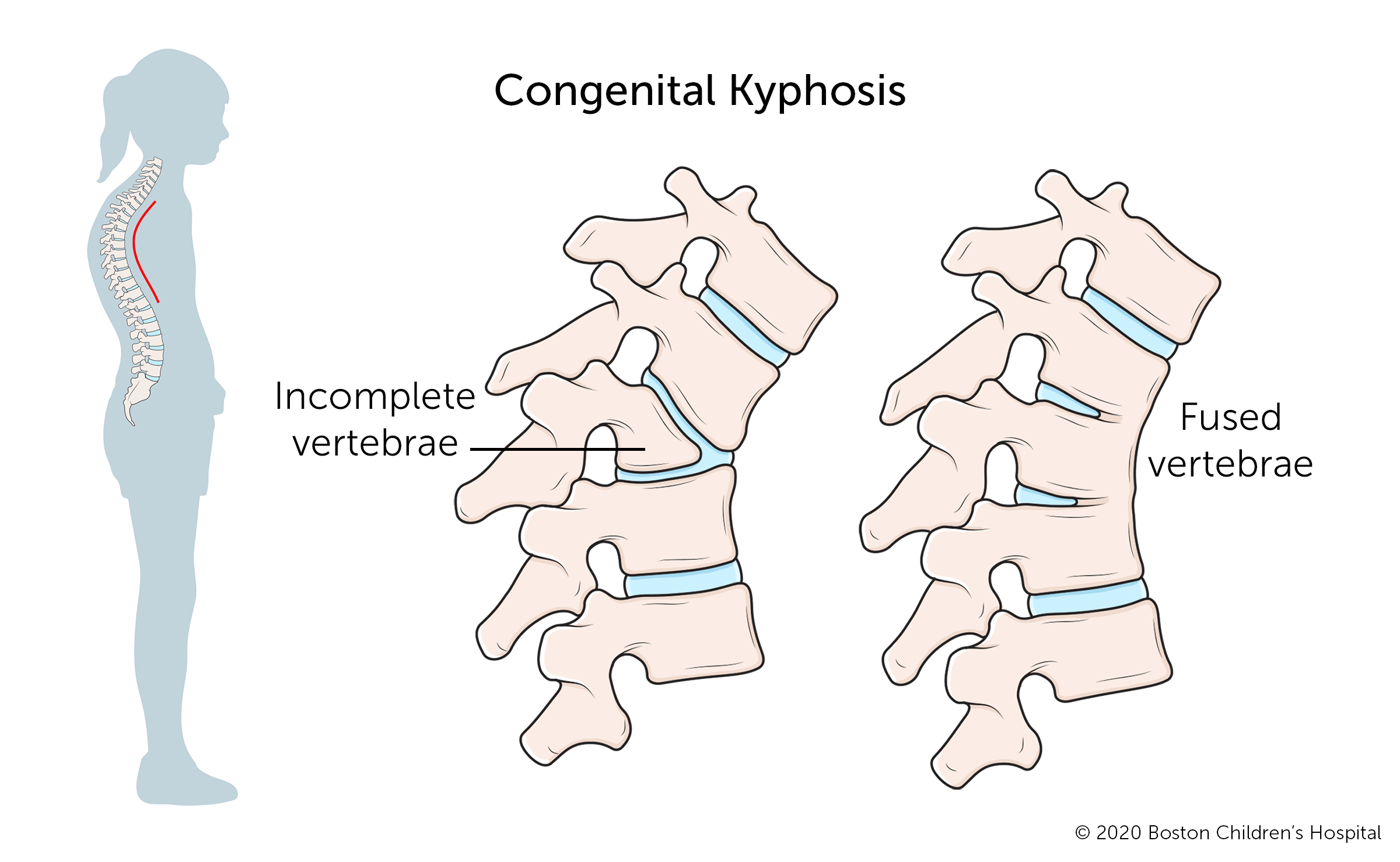
- your child has congenital kyphosis involving skeletal malformation (surgery may be needed at an early age)
- the kyphosis is caused by an infection or tumor
What is the long-term outlook for children with kyphosis?
When treated successfully, kyphosis can be corrected, and children go on to lead active, unrestricted lives. If your child needs surgery, they should be able to walk around in a few days and return home in about a week. They can go back to school within a month or so, and resume most activities within three to four months. Complete fusion takes about one year.