Pancreatitis | Symptoms & Causes
What are the symptoms of pancreatitis in children?
It is important to remember that the symptoms of pancreatitis can be vague and confused with signs of other diseases, such as viral gastroenteritis. If your child is an infant and cannot verbalize pain, they may be more fussy and irritable with persistent crying.
Acute pancreatitis symptoms
A child with acute pancreatitis needs immediate medical attention and will usually require hospitalization and close monitoring. Symptoms may include:
- abdominal pain
- nausea
- vomiting
- fever
- difficulty breathing
Chronic pancreatitis symptoms
The most common symptom of chronic pancreatitis is pain and discomfort in the upper abdomen — sometimes extending to the back — which may last hours or even days, and can be constant or intermittent. This pain may increase after eating and drinking.
Other symptoms include digestive issues such as:
- chronic weight loss, even when eating habits and amounts are normal
- nausea, vomiting, and/or diarrhea
- oily stools
What causes pancreatitis in children?
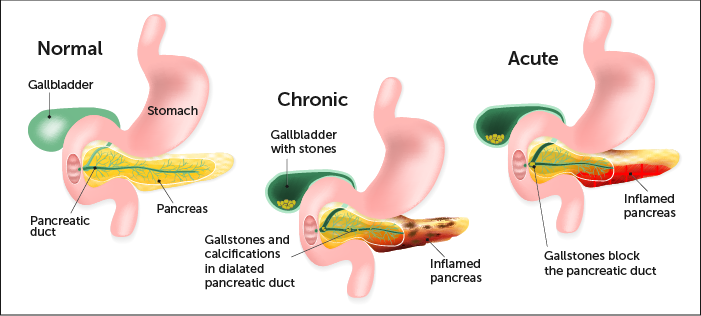
The pancreas is an organ located behind the stomach. It produces chemicals (called enzymes) needed to digest food. It also produces the hormones insulin and glucagon.
When scarring of the pancreas occurs, the organ is no longer able to make the right amount of these enzymes. As a result, your body may be unable to digest fat and key elements of food.
Damage to the parts of the pancreas that make insulin may lead to diabetes.
Causes of acute pancreatitis
There are many causes of acute pancreatitis, however, in approximately 30 percent of cases, a cause cannot be identified. Sometimes injury to the abdomen — such as a bicycle or playground accident or sports injury — can cause acute pancreatitis, or common medications and conditions, including:
- anti-seizure medications
- certain antibiotics
- specific types of chemotherapy
- gallstones or infections
- problems when the immune system attacks the body
- blockage of the tubes (ducts) that drain enzymes from the pancreas
- high levels of fats, called triglycerides, in the blood
- overactive parathyroid gland
Other chronic conditions may cause pancreatitis such as IBD, cystic fibrosis, or celiac disease.
Causes of chronic pancreatitis
Repeated episodes of acute pancreatitis can lead to chronic pancreatitis. In some cases, genetics may be a factor. However, sometimes, the cause is unknown.
Pancreatitis | Diagnosis & Treatments
How is pancreatitis in children diagnosed?
Acute pancreatitis
There is no single test to detect acute pancreatitis. The first step in the diagnosis process typically includes a blood test. This test will reveal whether there are abnormally high levels of enzymes, called amylase and lipase.
Imaging tests for acute pancreatitis may include:
- ultrasound examination
- magnetic resonance imaging scan, also known as an MRI
- computed tomography, also called a CT scan
Blood tests and radiology scans, such as ultrasound, CT, or MRI, may not always provide a clear-cut diagnosis. When this occurs, your doctor will make a clinical judgment based on your child’s history and the severity of symptoms.
Chronic pancreatitis
Unlike acute, a blood test generally does not identify chronic pancreatitis. Your clinician will perform variety of tests to determine if your child has chronic pancreatitis.
Imaging tests for chronic pancreatitis may include:
- Abdominal ultrasound: An ultrasound will indicate whether the pancreas is swollen or inflamed.
- Magnetic resonance imaging (MRI) scan: This can help rule out other causes of abdominal pain.
- Computed tomography (CT) scan: May also be used to help rule out other causes of abdominal pain.
- Endoscopic retrograde cholangiopancreatography (ERCP): A test that combines fluoroscopy (x-ray technique) with flexible endoscopy, involving a scope with a tiny high-definition camera on the end to see inside the body and help identify problems of the pancreas, pancreatic duct, liver, gallbladder, and bile ducts.
In some cases, imaging tests may not always provide a clear-cut diagnosis. When this occurs, your doctor will make a clinical judgment based on your child’s history and the severity of symptoms.
What are the treatment options for pancreatitis in children?
Acute pancreatitis
There is no specific medication or treatment that will help the pancreas to recover. Typically, what is required is supportive care to help the body’s normal functions.
Supportive care may include:
- providing medicine to help treat the pain.
- giving anti-nausea medications for persistent vomiting.
- administering intravenous fluids to ensure your child remains well hydrated.
- acetaminophen (such as Tylenol) can treat mild pain. However, stronger pain medication, such as narcotics like morphine, may be needed.
In cases of severe pancreatitis, causing a child to not eat for many days, your doctor may recommend giving essential liquid nutrition by placing a feeding tube through the nose into the stomach or intestine. Or they may recommend providing intravenous nutrition. Nutrition is important in the healing process.
Once the pain, vomiting, and discomfort associated with acute pancreatitis have resolved, your child’s appetite will slowly return. They should be encouraged to try and eat. You child’s diet will range from clear liquids to regular food. The choices will depend on what your child can tolerate.
Chronic pancreatitis
Currently, there is no specific medication or cure for chronic pancreatitis. However, many physicians offer supportive care in which they treat the symptoms in an effort to support the body’s normal function. Supportive care may include:
- medication to ease the pain associated with the condition
- provide pancreatic enzymes treatment which will help with digestion
- insulin may be given in severe cases to control the child’s sugar level
For children with chronic pancreatitis and pain, a surgical procedure called lateral pancreaticojejunostomy, or Peustow, may be recommended. This procedure connects a segment of the small intestine to the pancreas to improve drainage from the primary pancreatic duct. Another surgical option called a Total Pancreatectomy and Islet Auto Transplant (TPIAT) may be recommended. This complex procedure requires removing the pancreas and the hormone-producing cells, and isolating and returning the cells via injection into the patient’s liver.
How we care for pancreatitis
The Boston Children’s Hospital Pancreatic Disorders Program is recognized by the National Pancreas Foundation as a leader in the diagnosis and treatment of pancreatic disorders for children. Boston Children’s is ranked as one of the nation’s best children's hospitals by U.S. News & World Report. Our team includes the best gastroenterologists, hepatologists, and dietitians for children in the country — all dedicated to helping children with common or complex gastrointestinal, liver and nutritional problems. In addition, we have a close working relationship with the adult pancreatic center at Harvard Medical School-affiliated Brigham and Women’s Hospital, which helps us when it’s time to transition the care of young adults.


