Surgical management and decision-making for a traumatic growth plate injury
In 2011, a 6-year-old male sustained a traumatic lawnmower injury to his right leg. The initial injury was treated at another hospital in the patient’s home state, where it required numerous operations to clean the wound and remove injured tissue. The patient underwent a free flap and skin grafting in order to achieve coverage of the wound. He did have a bony injury to the femur, but it did not require operative fixation at the time.
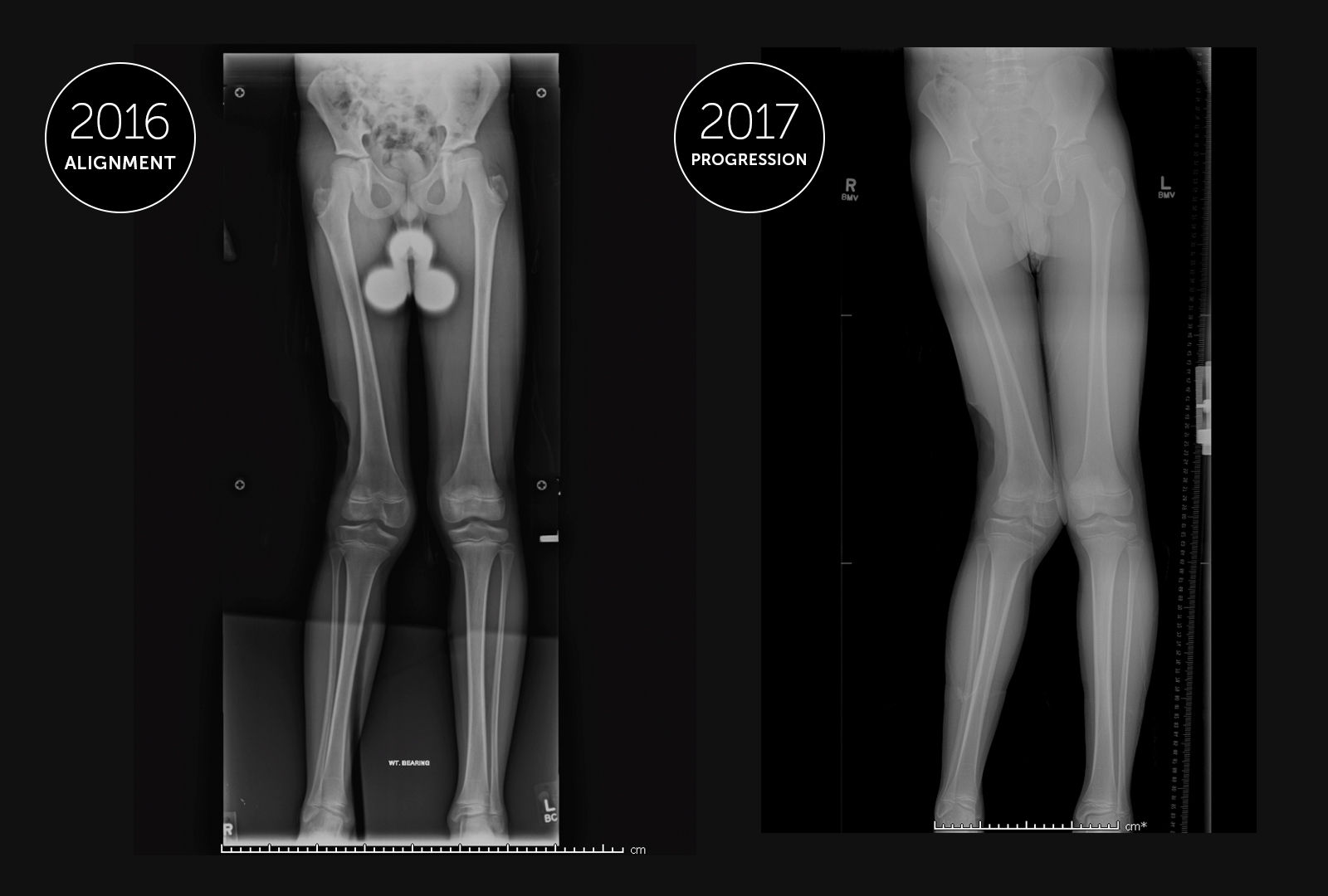
Six years later, at the age of 12, the patient came to the Lower Extremity Program at Boston Children’s Hospital after he began to develop a knock-kneed alignment of his right leg, resulting in a noticeable limp. Previously, he had been able to participate in sports and stay active, but now the limp was affecting him both physically and psychologically as it became more apparent.
Preoperative assessment
The patient’s mom reached out to Collin May, MD, MPH, a pediatric orthopedic surgeon in the Lower Extremity Program and Orthopedic Trauma Program at Boston Children’s, asking about potential management options for her son. Dr. May determined that, given the patient’s potential for growth, they could utilize this potential to improve the alignment of his leg.
First, May had to determine where the deformity was coming from. With the patient presenting a knock-kneed alignment, the deformity might have originated from the femur or the tibia. There was also the potential that there were secondary deformities elsewhere.
May analyzed the joint angles preoperatively on both the femur and tibia proximally and distally to assess where the deformity was located. Due to the patient’s history of trauma to the distal femur — and based on imaging showing the tibia was normally aligned — May determined that the deformity was resulting from the distal femur. The patient appeared to have a functioning distal femoral growth plate, with serial x-rays showing the bone increasing in length, however, it was growing more slowly on the lateral (out) side.
A straightforward procedure
The patient would therefore undergo a hemiepiphysiodesis procedure, in which a small plate and screws are placed spanning the growth plate on the medial (inside) of the patient’s distal femur. This allows for the lateral portion of the growth plate to continue growing, straightening the limb as the patient grows.
The procedure itself is relatively simple; involving a small incision, two screws and the plate. But much of the complexity in this case lies in the decision-making for both surgeon and family. Deciding when to remove the plate is seldom a straightforward process, and revolves around a number of factors.
Complexities of decision-making
Presuming the patient’s deformity corrects, May will have a discussion with the family about their options going forward. Generally, the plate is removed once the alignment of the limb is corrected (or slightly over-corrected), but it may have to be replaced if the deformity recurs. Another option once the limb is straight is to stop the growth of that growth plate completely through an epiphysiodesis procedure so the deformity doesn’t recur. This would then result in a leg length difference as the other leg continues to grow. The leg length difference could be managed by either lengthening the shorter side or performing an epiphysiodesis on the distal femoral physis of the other leg as well. Finally, if the deformity does not correct fully with the amount of growth remaining, it is possible that an osteotomy procedure will still be necessary to fully re-align the limb.
According to May, there isn’t one uniform decision for patient families. There is a lot that goes into the decision related to the risks of each operation, including the current height of the patient and their projected height at maturity. A patient likely to be shorter than average may not want to lose limb length through epiphysiodesis or limb shortening, so they may choose a limb lengthening procedure despite the greater risk and more involved recovery. Conversely, a patient who is likely to be taller at maturity may be more amenable to losing some height through an epiphysiodesis.
The array of options in the decision-making process is generally the most complex aspect of this type of case, and involves lengthy discussion with the patient family regarding which option may give their child a chance at the best outcome.
