Advanced instrumentation for atlantoaxial instability in a 2 year old child | Overview
In early 2018, a couple from Oklahoma adopted a 2-year-old female child with Down syndrome from China. Within one month of arriving in her new home, the child developed significant paralysis in all of her extremities. Physicians at a local hospital diagnosed atlantoaxial instability leading to compression and injury of the spinal cord. Between 10 and 20 percent of people with Down syndrome have atlantoaxial instability, largely due to the hyper-mobility of their joints and connective tissues, although the vast majority of cases are asymptomatic.
On the advice of physicians in Oklahoma, the child spent a week in traction followed by C1-C2 fusion surgery in February 2018. Post surgery, she was discharged in a halo vest that immobilized her cervical spine so the vertebrae could fuse. Five months after the surgery, the child’s cervical spine had not yet stabilized sufficiently to remove the halo vest.

Figure 2: CT scan showing severe upper cervical stenosis after instrumented fusion at outside hospital
Continued spinal cord injury
In November 2018, the parents contacted the Complex Cervical Spine Program at Boston Children’s Hospital. By then, the child had been hospitalized several times for recurrent pneumonia related to the spinal cord injury that prevented her diaphragm from working properly and interfered with her breathing. Orthopedic surgeon Daniel Hedequist, MD, talked with the parents by phone and reviewed radiological images that showed improperly fused vertebrae and spinal cord compression. He advised the parents that to restore neurologic function and prevent long-term problems, their daughter needed revision surgery to stabilize the spine and decompress the spinal cord.
The family decided to travel to Boston Children’s for the operation. The child was placed on the surgical schedule and the family made travel plans, however, the procedure had to be rescheduled twice due to the child’s recurring pneumonia and frequent hospitalizations. Finally, in January 2019, almost a year after the first surgery, Hedequist and Neurosurgeon-in-Chief, Mark Proctor, MD, performed revision surgery. As they had suspected, the C1 and C2 vertebrae were misaligned and the C1 vertebra was compressing the spinal cord. Despite the first surgery and halo vest, the spine was still not stable enough to support the skull and its movement continued to damage the spinal cord.
Surgical collaboration
During the first stage of the procedure, Proctor performed a C1 decompression, repositioning the bone so it no longer impinged on the spinal cord. Hedequist and Proctor then performed a skull-to-C2 fusion to stabilize the cervical spine. Using rigid screw rod and plating techniques, they attached a plate to the back of the child’s skull. Screws were then placed into the pedicles of the C2 vertebra and the plate was secured to the C2 vertebra with rods. Bone graft was then used from the patient’s iliac crest to maximize the chance of fusion.
Following surgery, the child spent a short time in the intensive care unit and was then transferred to a medical floor. The family returned to Oklahoma, where the patient is recovering. She will have to wear a halo for three months while the bones fuse and will wear a collar for two months once the halo is removed. Hedequist will collaborate with a surgeon in Oklahoma to manage the child’s follow-up care.

Figure 3: CT scan after decompression and instrumentation at BCH showing increased space for spinal cord
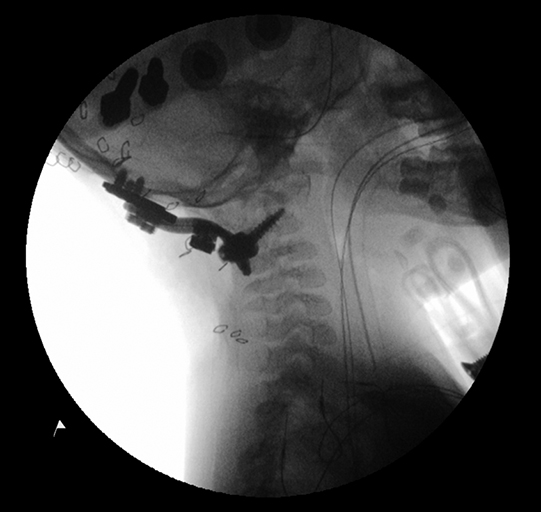
Figure 4: Fluoroscopy view showing occipital plate and C2 pedicle screw construct
Better fusion rates and deformity correction
While rigid screw rod and plating techniques are commonly used on teenage and adult patients, smaller children have traditionally been instrumented with wires to stabilize the spine. However, our experience and clinical research shows that when performed well, modern instrumentation is feasible on children as young as 2 years old and has better results in terms of fusion rates, deformity correction and less stringent immobilization requirements.
Given the catastrophic risks of spinal surgery at the upper cervical spine, including stroke, quadriplegia and death, another important component of this case was the active involvement of both a neurosurgeon and orthopedic surgeon. Particularly for high-complexity cases, the collaboration of two experienced attending physicians with complementary skill sets is essential to ensure patient safety.

